THE ROLE OF DIETARY PATTERNS IN MENTAL HEALTH.
The Role of Dietary Patterns in Mental Health
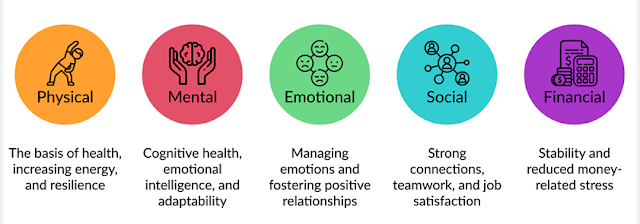
Mental health is a complex and intricate part of our overall well-being, influenced by a variety of factors such as genetics, environment, lifestyle choices, and eating habits. Recently, probing has increasingly highlighted the crucial role nutrition plays in mental health, revealing how our food choices can affect not just our physical health but also our emotional and cognitive states. Historically, mental health has been primarily addressed through psychological, social, and sometimes medical approaches, often overlooking the significance of diet. However, growing evidence suggests that dietary patterns are vital in preventing, managing, and treating mental health issues like depression, anxiety, and stress. As we learn more about the connection between the gut and brain and its impact on mood and thinking, it becomes evident that our eating habits can significantly influence our emotional stability, cognitive abilities, and overall mental health.
Recent studies highlight the importance of the gut-brain axis, which is the communication pathway between the gut and the brain. This connection plays a crucial role in how our diet influences mood and mental well-being. The gut is home to trillions of bacteria that help produce neurotransmitters like serotonin and dopamine, which are essential for regulating mood, emotions, and cognitive functions. In fact, around 90% of serotonin, a key neurotransmitter for mood stability is generated in the gut. Thus, keeping a healthy gut microbiome is vital for maintaining good mental health. Consuming a diet rich in fiber, prebiotics, and probiotics found in fruits, vegetables, whole grains, and fermented foods can foster a diverse and balanced microbiota. This diversity supports the creation of beneficial metabolites that positively impact brain function and mood. On the other hand, diets high in processed foods, refined sugars, and unhealthy fats can upset the microbiome's balance, potentially leading to mental health issues like depression, anxiety, and cognitive decline.
There is growing evidence that specific dietary habits can significantly impact brain health, with the Mediterranean diet being one of the most researched and advocated for its positive effects on mental well-being. This diet is abundant in fruits, vegetables, whole grains, legumes, nuts, and seeds, along with healthy fats, especially olive oil. Studies have indicated that it can offer protective benefits against various mental health issues. The Mediterranean diet is rich in omega-3 fatty acids, antioxidants, polyphenols, and vitamins, all of which can help lower inflammation and oxidative stress in the brain factors associated with depression and cognitive decline. Omega-3 fatty acids, particularly found in fatty fish like salmon, mackerel, and sardines, are especially advantageous for brain health. They enhance neuronal function, reduce inflammation, and have been shown to ease symptoms of depression and anxiety. The antioxidants from the fruits and vegetables in this diet help shield brain cells from oxidative damage, while polyphenols found in olive oil, wine, and other plant-based foods further support neuroprotection and cognitive function. This dietary approach has been associated with a lower risk of depression, anxiety, and cognitive decline, highlighting the important role that our food choices can play in maintaining mental health.
Diets that are rich in processed foods, refined sugars, and unhealthy fats hallmarks of the Western diet have been associated with a higher risk of mental health problems. This typical diet, filled with processed snacks, sugary drinks, fried foods, and red meats, can lead to inflammation and oxidative stress, both of which are harmful to the brain. Inflammation in the brain plays a significant role in the onset of mental health disorders like depression and schizophrenia. Eating Trans fats and too much sugar triggers an inflammatory response in the body, and ongoing inflammation can interfere with brain function and emotional stability. Additionally, a high sugar diet can lead to fluctuations in blood sugar levels, resulting in mood swings, irritability, and fatigue common signs of anxiety and depression. The Western diet also disrupts the gut microbiome, which can hinder communication between the gut and brain, potentially worsening mental health issues.
The influence of diet on mental health goes beyond merely preventing disorders; it also plays a crucial role in treatment and management. An increasing number of clinical studies indicate that changes in diet can lead to significant enhancements in mental health. For example, research found that people suffering from depression who adopted a nutrient-dense diet rich in whole foods and healthy fats saw considerable improvements in their symptoms. Additionally, omega-3 supplements have shown effectiveness in alleviating symptoms of depression and anxiety, especially in individuals with low levels of these vital fatty acids. These results underscore the potential of dietary strategies as complementary options to conventional psychological treatments and medications, promoting a more comprehensive approach to mental health care.
The idea of "food as medicine" is gaining traction in the realm of mental health. Ongoing research is uncovering the connections between our diets and mental well-being, suggesting that making dietary adjustments could be an effective way to address issues like depression, anxiety, and stress. However, it's essential to understand that diet isn't a standalone solution. Mental health is affected by numerous factors, such as genetics, environment, and individual experiences, so any dietary changes should be part of a more comprehensive approach to overall mental health. Nevertheless, the increasing evidence highlights the significant impact that our food choices have on our emotional and cognitive well-being, making a nutrient-dense diet a valuable strategy for both preventing and managing mental health challenges.
Dietary habits play a crucial role in mental health, affecting both the prevention and management of mental health issues. Consuming a balanced diet rich in whole foods, healthy fats, and vital nutrients can enhance gut health, lower inflammation, and boost brain function, which in turn supports better mood stability and cognitive abilities. On the other hand, diets that are high in processed foods, added sugars, and unhealthy fats can impair brain function and lead to mental health challenges. The increasing awareness of the gut-brain connection and the importance of certain nutrients in mental health open up new avenues for preventing and treating conditions such as depression and anxiety. As we delve deeper into the intricate link between diet and mental health, it becomes more evident that nutrition is a fundamental component of overall mental wellness.
The Gut-Brain Connection: A Key Relationship
The gut-brain connection is a fascinating and intricate communication network that links the gastrointestinal system with the brain, playing a crucial role in both our physical and mental well-being. Newly, the importance of this connection has come to the forefront, especially regarding mental health. Research has increasingly shown that the gut and brain interact in ways that can affect our mood, behavior, and cognitive abilities. Disruptions in this communication can lead to various mental health issues. This complex system operates through multiple pathways neural, hormonal, and immunological enabling signals to travel in both directions, impacting not just digestion but also emotional balance and mental health. Gaining insight into how the gut-brain connection works is vital for understanding how our diet and nutrition can significantly influence mental health outcomes.
The gut-brain axis relies heavily on the vagus nerve, which is the longest cranial nerve stretching from the brainstem to the abdominal organs. This nerve facilitates communication in both directions, enabling the brain to affect digestive functions while also allowing the gut to relay information back to the brain. Approximately 90% of the fibers in the vagus nerve are afferent, meaning they carry sensory information from the gut to the brain. These signals can impact brain activity, influencing mood, cognitive abilities, and emotional reactions. For example, the gut microbiota, consisting of trillions of bacteria and other microorganisms in the digestive system, produces various metabolites that can alter brain chemistry. Through the vagus nerve, these microbial metabolites like short-chain fatty acids (SCFAs) can reach the brain and affect the production of neurotransmitters such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), which are crucial for mood regulation, behavior, and cognitive function. This bidirectional communication between the gut and brain is fundamental to the gut-brain axis and plays a significant role in understanding the links between diet, gut health, and mental well-being.
The gut-brain axis is shaped not just by neural connections but also by hormonal messages from the endocrine system. A key player in this communication is cortisol, often referred to as the "stress hormone." Its levels change in response to stress, impacting both gut and brain functions. For example, chronic stress can disrupt the gut microbiome, encouraging harmful bacteria to thrive while diminishing beneficial ones, resulting in dysbiosis, which is an imbalance of gut bacteria. This condition has been linked to various mental health problems, such as anxiety, depression, and cognitive decline. Additionally, the gut produces several hormones that affect the brain, including ghrelin, which plays a role in appetite and mood, and leptin, which helps regulate energy balance and has been associated with depression. These hormonal interactions highlight the two-way relationship of the gut-brain axis, where the health of the gut can affect brain function and vice versa.
The immune system plays a crucial role in the gut-brain axis. A large number of the body's immune cells reside in the gut, which acts as a primary defense against harmful pathogens. The gut microbiota plays a crucial role in managing immune responses. When there's an imbalance, called dysbiosis, it can result in heightened intestinal permeability, commonly known as "leaky gut."When the gut lining is damaged, harmful substances like endotoxins can seep into the bloodstream, causing systemic inflammation. This ongoing low-level inflammation has been associated with various mental health issues, such as depression and anxiety. Research has indicated that individuals with mental health disorders often have elevated levels of inflammatory markers, like cytokines, pointing to a possible link between inflammation and the development of these conditions. By impacting the immune system, the gut microbiome can indirectly influence brain function and may play a role in the emergence or worsening of mental health challenges.
Research into the gut-brain connection is revealing just how significantly the gut microbiome can affect mental health. Evidence suggests that an imbalance in gut bacteria, known as dysbiosis, may play a role in the onset of mood disorders like anxiety and depression. For instance, people suffering from depression often exhibit a notably altered gut microbiome, characterized by lower diversity in microbial species and a higher presence of pro-inflammatory bacteria. This imbalance is believed to exacerbate depressive symptoms by increasing inflammation and disrupting communication between the gut and the brain. On the other hand, a healthy and varied microbiome is linked to improved emotional regulation, cognitive abilities, and resilience against stress. In studies with animals, modifying the gut microbiota using prebiotics or probiotics has been shown to affect stress and anxiety-related behaviors, reinforcing the idea that gut health is essential for mental well-being.
The link between the gut and the brain is especially important when we think about how our diet affects mental health. What we eat can significantly change the makeup of our gut microbiome, which in turn can impact our mental well-being. Diets that are high in fiber, prebiotics, and probiotics like the Mediterranean diet have been found to foster a healthy microbiome that benefits both brain health and emotional stability. Conversely, diets loaded with processed foods, refined sugars, and unhealthy fats can throw off the balance of gut bacteria, leading to dysbiosis and possibly contributing to mental health challenges. Additionally, certain nutrients such as omega-3 fatty acids, B vitamins, and antioxidants play a role in both gut health and brain function, highlighting the crucial role of nutrition in supporting the gut-brain connection.
In recent years, the exploration of the gut-brain connection has unveiled exciting new avenues for therapeutic approaches aimed at enhancing mental well-being. For instance, the use of probiotics and prebiotics has shown potential in restoring a balanced microbiome and reducing symptoms associated with depression, anxiety, and various mood disorders. Probing found that individuals with depression experienced notable improvements in their mood and anxiety levels after taking probiotic supplements. Likewise, prebiotics, which nourish beneficial gut bacteria, have been linked to increased production of short-chain fatty acids (SCFAs) that promote brain health. These insights indicate that focusing on the gut microbiome through dietary changes could be a valuable strategy for both preventing and addressing mental health issues.
The gut-brain axis plays a vital role in mental health, with the state of our gut significantly impacting mood, behavior, and cognitive abilities. This intricate communication system, which includes neural, hormonal, and immune pathways, is heavily influenced by the gut microbiome, shaped by our dietary choices and lifestyle habits. As research into this connection advances, it becomes increasingly evident that what we eat and the condition of our gut microbiota are essential for maintaining mental wellness. This emerging knowledge holds important implications for both the prevention and treatment of mental health issues, suggesting new strategies that prioritize gut health to enhance mental well-being.
The Mediterranean Diet: A Shield for Mental Well-Being
The Mediterranean diet, well-known for its advantages to physical health, is gaining recognition for its possible protective benefits for mental well-being. This eating style, traditionally embraced by those in the Mediterranean region, focuses on a variety of plant-based foods, healthy fats, and moderate amounts of fish and poultry, while minimizing red meat and processed items. Packed with fruits, vegetables, whole grains, legumes, nuts, seeds, and olive oil, the Mediterranean diet provides a rich source of nutrients that enhance overall health, including specific elements that support brain function, emotional balance, and cognitive abilities. Numerous studies indicate that following this diet may lower the risk of mood disorders such as depression, anxiety, and cognitive decline, making it an excellent dietary approach for fostering mental health.
One of the standout features of the Mediterranean diet is its abundant omega-3 fatty acids, especially those derived from fish and seafood. These essential fats are vital for maintaining brain structure and function, affecting both the physical makeup of brain cells and how neurotransmitters operate. Probing indicates that omega-3s can help reduce inflammation and oxidative stress, factors often linked to mood disorders such as depression. Evidence suggests that taking omega-3 supplements can ease symptoms of depression and anxiety, particularly in those who have low levels of these important fats. The Mediterranean diet includes fatty fish like salmon, mackerel, and sardines, which are excellent sources of omega-3s, making them crucial for brain health. Incorporating these foods regularly into your diet can help safeguard against mental health challenges by enhancing cognitive function and emotional stability.
The Mediterranean diet is not only rich in omega-3 fatty acids but also packed with antioxidants, especially polyphenols, which are abundant in fruits, vegetables, nuts, and olive oil. These plant-based compounds are known for their strong anti-inflammatory and antioxidant effects, helping to shield the brain from oxidative stress and lower inflammation factors often associated with mood disorders like depression. Studies indicate that these antioxidants can boost cognitive function, elevate mood, and guard against cognitive decline as we age. For example, the polyphenols in olive oil, a key element of the Mediterranean diet, have been found to enhance brain health by decreasing the production of inflammatory molecules and encouraging the growth of brain-derived neurotrophic factor (BDNF), a vital protein for neuron health and survival. By supplying the brain with a consistent flow of these protective compounds, the Mediterranean diet supports mental resilience and lowers the likelihood of developing mental health issues.
The Mediterranean diet emphasizes whole foods, high fiber, and nutrient-rich options, all of which are vital for maintaining gut health. This, in turn, significantly impacts mood and cognitive abilities through the gut-brain connection. A fiber-rich diet that includes fruits, vegetables, legumes, and whole grains promotes a diverse and thriving microbiome, which is associated with better mental well-being. The gut microbiome generates short-chain fatty acids (SCFAs) like butyrate, known for their role in enhancing brain function by lowering inflammation and boosting neurotransmitter production, including serotonin, a key mood regulator. Research indicates that those who adhere to a Mediterranean-style diet tend to have a more varied and balanced gut microbiome, potentially explaining some of its mental health benefits. By fostering the growth of beneficial gut bacteria, this diet may contribute to improved mood, alleviation of anxiety and depression symptoms, and enhanced cognitive abilities.
The Mediterranean diet also highlights the role of moderate red wine consumption, which may play a part in its mental health advantages. Red wine contains polyphenols, including resveratrol, known for their neuroprotective properties. While it's widely recognized that heavy drinking can harm mental health, enjoying one to two glasses of red wine daily may lower the risk of depression and cognitive decline, likely thanks to its antioxidant and anti-inflammatory effects. Some research indicates that moderate alcohol intake could boost the production of neurotransmitters like serotonin, which can improve mood and encourage relaxation. It's essential to remember that the mental health benefits linked to wine are primarily attributed to its polyphenols and should be viewed as part of a comprehensive healthy eating approach.
The Mediterranean diet offers protective benefits for mental health that extend beyond just its nutritional content; the lifestyle that accompanies this way of eating is also vital for enhancing emotional well-being. In Mediterranean societies, meals are typically enjoyed in a social setting, surrounded by family and friends. This focus on shared dining experiences and social bonds contributes to psychological advantages that can alleviate stress and create a sense of community and support. Additionally, the Mediterranean way of life is generally less stressful, emphasizing physical activity and outdoor time, both of which are essential for mental wellness. Engaging in regular exercise has been proven to lessen symptoms of depression and anxiety, boost cognitive abilities, and improve overall mood. Therefore, when integrated into a holistic lifestyle, the Mediterranean diet not only supplies key nutrients for brain health but also promotes social engagement and physical fitness two vital elements for building mental resilience and emotional stability.
There is an increasing amount of research highlighting the mental health advantages of the Mediterranean diet, as shown in various large cohort studies and clinical trials. For instance, a 2017 study published in The Lancet Psychiatry revealed that people who followed a Mediterranean-style diet had a notably lower risk of developing depression compared to those who adhered to a typical Western diet, which tends to be rich in processed foods, refined sugars, and unhealthy fats. Additionally, another study indicated that individuals on the Mediterranean diet reported better moods and lower levels of anxiety and stress. These results imply that the Mediterranean diet could not only help prevent mental health issues but also act as a supportive treatment for those already facing anxiety, depression, and cognitive decline.
The Mediterranean diet serves as a beneficial dietary approach for mental health, thanks to its diverse range of nutrients like omega-3 fatty acids, polyphenols, and fiber.
Nutritional Shortfalls and Their Effects on Mental Well-Being
Nutritional shortfalls are increasingly acknowledged as key factors contributing to various mental health issues, influencing both cognitive abilities and emotional stability. The link between what we eat and our mental health is intricate, with certain nutrients being vital for the brain's structure, function, and chemical processes. Lacking essential vitamins, minerals, fatty acids, and amino acids can deeply impact mental health, potentially leading to or worsening conditions like depression, anxiety, cognitive decline, and even more serious neuropsychiatric disorders. This relationship underscores the necessity of a well-rounded and nutrient-dense diet for supporting optimal mental health, as even slight deficiencies can lead to notable effects on mood, thinking, and behavior.
One of the most extensively researched nutritional deficiencies linked to mental health challenges is the shortage of B vitamins, especially folate (B9), B12, and B6. These vitamins are vital for producing neurotransmitters such as serotonin, dopamine, and norepinephrine, which are crucial for regulating mood, cognitive function, and emotional reactions. When any of these vitamins are deficient, it can disrupt the balance of these neurotransmitters, leading to issues like depression, irritability, fatigue, and cognitive difficulties. For example, low folate levels have been associated with depression and cognitive decline, and studies indicate that people with insufficient folate may not respond as well to antidepressant treatments. Likewise, a deficiency in vitamin B12, essential for nerve health and red blood cell production, can result in mood swings, cognitive issues, and in severe cases, psychosis. Additionally, insufficient B6, which plays a role in synthesizing serotonin and GABA, can also lead to anxiety and depression. These deficiencies are particularly common among groups with poor dietary habits, such as the elderly, those on restrictive diets, or individuals with gastrointestinal disorders that hinder nutrient absorption.
One important nutrient that significantly influences mental health is vitamin D. Often referred to as the "sunshine vitamin," vitamin D is synthesized in the skin when exposed to sunlight and can also be found in certain foods like fatty fish, fortified dairy products, and egg yolks. This vitamin is essential for proper brain function, as it helps regulate the genes that are involved in neurotransmitter production and inflammation. Studies have indicated that low vitamin D levels are closely linked to a higher risk of depression and various mood disorders. Research has shown that people with low serum vitamin D are more prone to experiencing depressive symptoms, and taking vitamin D supplements can enhance mood in those who are deficient. Furthermore, vitamin D's ability to reduce inflammation and promote neuroplasticity highlights its vital role in supporting mental well-being. Given that vitamin D deficiency is prevalent, especially in areas with limited sunlight or among those who spend a lot of time indoors, maintaining adequate levels through diet and supplementation is crucial for mental health.
The significance of omega-3 fatty acids in mental health is a topic of great interest. Omega-3s, especially eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are vital polyunsaturated fats found in sources like fatty fish, flaxseeds, and walnuts. These fatty acids play a crucial role in the structure of brain cell membranes and are involved in various brain functions, such as neurotransmission, managing inflammation, and preserving neuronal health. Research has shown that a lack of omega-3s is associated with a higher risk of mood disorders, including depression, anxiety, and bipolar disorder. Insufficient omega-3 levels can lead to decreased serotonin production and other neurotransmitters, along with increased brain inflammation, both of which can lead to mental health challenges. Studies indicate that omega-3 supplementation can have antidepressant and anti-anxiety effects, enhancing mood and cognitive abilities in those who are deficient. In areas where fish intake is low or omega-3s are not commonly included in the diet, like many Western nations, supplementation could be a beneficial approach for preventing and addressing mental health issues.
Mineral deficiencies, especially in magnesium, zinc, and iron, significantly impact mental health. Magnesium is vital for many brain functions, such as managing neurotransmitter activity, supporting synaptic plasticity, and handling stress responses. Low levels of magnesium have been associated with heightened anxiety, irritability, and sleep issues, while magnesium supplements have shown potential in reducing anxiety and depression symptoms. Zinc is crucial for regulating brain signaling pathways and is important for mood stability. A lack of zinc has been linked to both depression and anxiety, with research indicating that zinc supplements may have antidepressant benefits. Iron deficiency, which is particularly common in women of childbearing age and children, can cause cognitive issues and fatigue. Iron is necessary for transporting oxygen and producing energy, and its deficiency can lead to difficulties in concentration, irritability, and depressive feelings. Maintaining a balanced diet rich in these essential minerals is key to supporting mental health and preventing cognitive and emotional challenges.
A nutrient that is gaining recognition for its role in mental health is iodine. This essential element is crucial for producing thyroid hormones, which play a key role in regulating metabolism, growth, and brain function. When there is a deficiency of iodine, it can lead to thyroid issues, manifesting as symptoms like fatigue, cognitive decline, depression, and in severe cases, cretinism, which is a type of intellectual disability. In regions where iodine deficiency is common, such as certain areas in sub-Saharan Africa and Southeast Asia, studies have shown that iodine supplementation can enhance cognitive abilities and overall mental health, especially in children. Even a mild lack of iodine can result in subtle cognitive challenges, underscoring the necessity of sufficient iodine intake, particularly during pregnancy and early childhood, when the brain is most vulnerable to nutritional factors.
Poor dietary habits, particularly those involving high levels of processed foods, refined sugars, and unhealthy fats, can significantly increase the risk of mental health issues. Research indicates that diets high in refined sugars and trans fats can lead to systemic inflammation, oxidative stress, and changes in brain function, all of which may contribute to mood disorders. Additionally, these unhealthy eating habits can harm the gut microbiome, disrupting the communication pathways between the gut and brain that are essential for regulating mood and cognitive function. On the other hand, diets abundant in fruits, vegetables, whole grains, and healthy fats are linked to better mental health outcomes, as these foods promote brain health through their anti-inflammatory, antioxidant, and microbiome-supporting properties.
Nutritional deficiencies are a crucial yet often neglected aspect of mental health issues. Key nutrients like B vitamins, omega-3 fatty acids, vitamin D, magnesium, zinc, and iodine are vital for proper brain function, neurotransmitter balance, and emotional stability. Lacking these nutrients can contribute to or worsen mental health challenges such as depression, anxiety, and cognitive decline. It's important to ensure a well-rounded diet that provides these essential nutrients to support mental wellness and help prevent mental health disorders. In situations where diet alone isn't enough or absorption is an issue, supplements may be needed to bring nutrient levels back to where they should be, ultimately enhancing mental health outcomes. Therefore, tackling nutritional deficiencies is an essential part of mental health care and prevention, highlighting the significant role of good nutrition in fostering emotional and cognitive well-being.
The Impact of the Western Diet on Mental Health
The Western diet, which is marked by a high intake of processed foods, refined sugars, unhealthy fats, and a scarcity of fruits, vegetables, and whole grains, has been increasingly associated with various mental health challenges, such as depression, anxiety, and cognitive decline. This eating pattern, prevalent in many developed countries, not only harms physical health but also seems to have considerable adverse effects on mental well-being. Research has indicated that the Western diet's focus on high glycemic index foods, trans fats, and artificial additives leads to inflammation, oxidative stress, and disruptions in the gut microbiome, all of which are linked to the onset and worsening of mental health issues.
One major factor contributing to mental health challenges linked to the Western diet is its excessive amount of refined sugars and carbohydrates. Diets that are high in sugary snacks and drinks, along with refined carbs like white bread and pasta, can cause quick spikes and drops in blood sugar levels. These fluctuations may result in episodes of high blood sugar followed by sudden decreases, which can lead to mood swings, irritability, and tiredness. Additionally, a diet loaded with sugar and refined carbs can trigger systemic inflammation and disrupt brain function. Studies indicate that high sugar intake can boost the production of pro-inflammatory cytokines, which play a role in the immune response. Chronic low-grade inflammation is increasingly seen as a significant contributor to mood disorders, including depression. Inflammation in the brain can hinder the function of neurotransmitters, especially serotonin, which is vital for mood regulation and emotional well-being. Therefore, following a Western-style diet that is rich in processed sugars and refined carbohydrates may play a role in the development and intensity of depression and anxiety.
One important factor of the Western diet is its significant consumption of unhealthy fats, especially trans fats and omega-6 fatty acids, which are prevalent in fast food, baked goods, and processed snacks. These types of fats can lead to inflammation, particularly when they are consumed in high amounts compared to omega-3 fatty acids, which are known for their anti-inflammatory benefits. Inflammation in the brain can interfere with neural communication and may play a role in the onset of mood disorders. Research indicates that a high intake of trans fats is linked to a greater risk of depression and cognitive decline. Unlike the healthy fats found in sources such as fish and nuts, trans fats can elevate oxidative stress levels in the brain, resulting in damage to brain cells and impairing normal brain function. On the other hand, diets rich in omega-3 fatty acids, found in foods like fatty fish and flaxseeds, have demonstrated antidepressant and neuroprotective properties, underscoring the importance of maintaining a balanced ratio of fats in our diet.
All rights reserved by Bubble Organic © 2024